The most severe pain is believed to be toothache. Although the same can be said for ear pain and headaches. Joint pain is no exception. It can make a person suffer, deprive them of sleep and appetite.
The pain is sharp or dull, throbbing, aching, at night or throughout the day - all symptoms of joint diseases.
Prevalence of joint pain
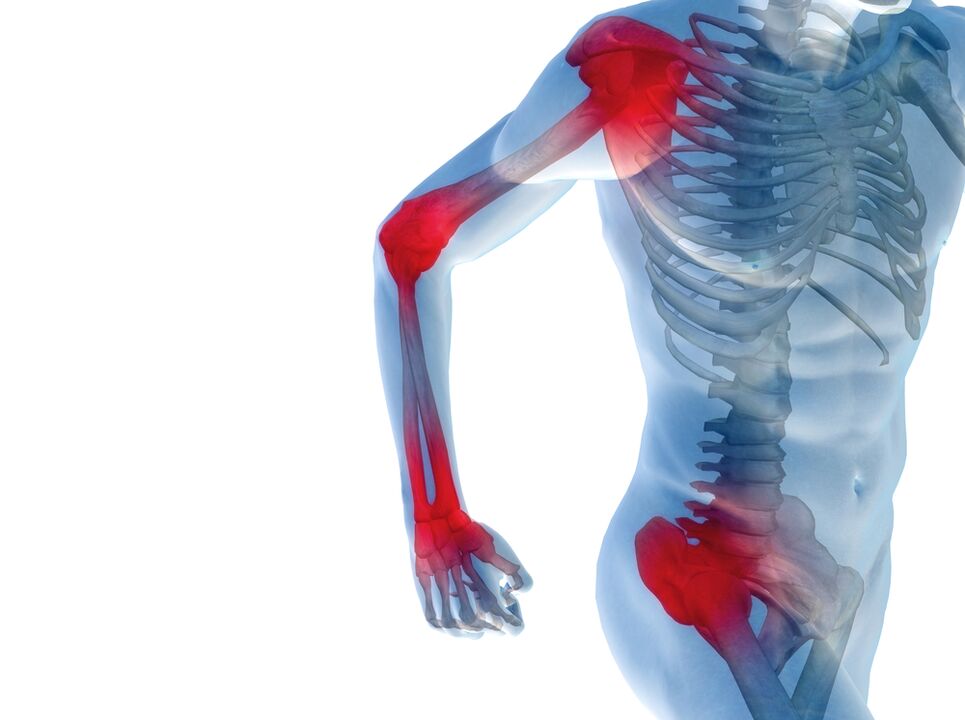
There is no clear trend between the severity of joint pain and its prevalence. The knee joint can hurt more than the shoulder, elbow and hand at the same time. Sensations in the spine may be painful with generalized osteochondrosis or ankylosing spondylitis. But most often people are bothered by pain in the extremities.
The arms and legs undergo significant stress throughout life: weight, action, injuries. Pain, joint pain and their deformation inevitably accompany age-related changes in the musculoskeletal system.
Pain mechanism

Why joints hurt is a question that even a doctor finds difficult to answer unequivocally.
The mechanism of pain when the musculoskeletal system is damaged is quite complex. Most often, these symptoms are caused by the following processes:
- Inflammation of the joints, or polyarthritis.The inflammation itself triggers the production of substances that can cause pain. Additionally, they increase the sensitivity of pain receptors to repeated exposure. That is why the usual load on the inflamed joint leads to a sharp painful reaction.
- Swelling of the joint.Its increase in volume resembles a joint tumor. Edematous tissues mechanically exert pressure on the joint structures, causing discomfort and worsening the severity of the process.
- Dystrophic changes.This is what we call bone and cartilage wear and tear. With age and constant stress, joint function deteriorates. The production of synovial fluid is disrupted and sliding of the joint surfaces becomes difficult. Their constant irritation by friction stimulates the growth of the subchondral bone. Such marginal bony growths are called osteophytes and can cause real suffering to a person. They look like protruding bumps on the joints. Osteophytes are often injured, which causes their inflammation, thus completing the pathological circle.
- Trauma and post-traumatic complications.Serious injuries: bruises, dislocations, fractures do not disappear without a trace. Even if the damage is healed, joint pain and stiffness may persist for the rest of your life. Doctors often complain of aching pain in damaged joints. They usually get worse when the weather changes or at night.
- Trade disruptions.Calcifications are deposited in tendons and ligaments due to metabolic disorders. Their violation leads to acute pain syndrome.
These pathological processes in the joints develop in diseases of the musculoskeletal system.
Diseases of the musculoskeletal system
The number of joint diseases is significant. There are rare forms, isolated throughout the world, and there are also those found in most people. The prevalence of these diseases explains why every person suffers from joint pain at least occasionally.
It is important to know the main diseases of the musculoskeletal system, so as not to ignore dangerous symptoms, but to start treating and curing the disease in time.
Osteoarthritis
Doctors constantly hear from elderly patients that they experience pain in the joints of their arms and legs, lower back, and neck. In addition to pain, they complain of joint deformities, difficulty walking and the inability to do their homework.
These symptoms are characteristic of osteoarthritis of the joints. In the case of deformation of bones and cartilage, we speak of deforming osteoarthritis. Severe deforming osteoarthritis can render a person completely disabled.
Osteoarthritis affects all joints, large and small. It is only important that they experience enough stress.
If you overload the joints, osteoarthritis will develop several years earlier, especially if there are predisposing factors. These include:
- Constant load. It can be redundant or monotonous. Static loads play an important role in the development of osteoarthritis changes.
- Hypothermia or overheating.
- Injuries - bruises and fractures, subluxations and dislocations.
- Overweight. Obesity is one of the most important risk factors for the development of osteoarthritis deformans.
- Bad nutrition.
- Lack of movement.
- Infections and subsequent inflammation of the joints are polyarthritis.
Degenerative diseases of the shoulder girdle

The shoulder joint is the most mobile joint in the body, with the maximum range of motion. It supports dynamic loads, so degenerative changes in the structures of the shoulder girdle are rare.
They usually develop in old age. Marginal bony growths appear and atrophy of the articular cartilage. If degenerative changes in the shoulder joint are pronounced, the cause should be investigated. This usually occurs due to a fracture or osteochondromatosis.
Pain in the shoulder joints is aching and constant; stiffness is often associated with degenerative changes in adjacent structures:
- Deposition of calcifications in the supraspinatus tendon and the resulting painful arc of abduction syndrome. With this pathology, pain in the joints occurs when trying to move the shoulder along a certain arc. If you change the angle of inclination, the pain disappears.
- Frozen shoulder syndrome. This condition is characterized by severe stiffness of the shoulder girdle. Occurs as a result of prolonged immobilization of the shoulder - when applying a bandage, providing rest to the arm affected by thoracic radiculitis.
No pronounced deformation of the elements of the shoulder girdle is observed. Symptoms and complaints associated with damage to adjacent structures, rather than deforming osteoarthritis of the shoulder, usually come first.
Osteoarthritis of the elbow joint
The likelihood of developing degenerative changes in the elbow joint is low. It increases with old age and among people in certain professions. Monotonous physical activity has a negative impact on joint processes, especially when exposed to vibration.
Deforming osteoarthritis of the elbow region is common among tennis players, masons and miners, blacksmiths and foundry workers.
Usually the pain in the joints is dull, aching and intensifies with exercise. No significant deformation of the joints is observed. Sometimes, under the influence of provoking factors, inflammation of the joints also joins osteoarthritis, painful swelling appears in the elbow area and the pain bothers you even when resting.
Deforming osteoarthritis of the hands and finger joints
In recent years, the diagnosis of osteoarthritis of the hands has become the answer to the question of why the finger joints hurt at a young age. This disease rejuvenates quickly. Already at the age of 30-35, with complaints of pain in the finger joints, signs of deforming osteoarthritis of the first degree can be seen on an x-ray. The reasons are varied:
- The number of professions that put pressure on the joints of the hands and fingers is increasing: programmers, typists and simply active computer users. And it is especially young people who are involved in this process.
- Work in hypothermic conditions. These are tram and trolleybus drivers in winter, builders and villagers.
- Lack of normal dynamic loads on the finger joints. Few people strive to do gymnastics, especially therapeutic exercises.
- Concomitant diseases - inflammation of the joints.
The joints of the fingers and hands become deformed over time and an inflammatory tumor can be detected in the phalanges with the development of polyarthritis. Movements become painful and difficult. Joint pain is intermittent at first, then becomes constant, dull or aching.
Degenerative foot diseases
Leg joints are more susceptible to degeneration, because their main load is static. Weight and static loads are the main causes of the development of osteoarthritis deformans of the legs. In this area it appears in the following forms:
- Damage to the hip joints – coxarthrosis.
- Damage to the knees with the formation of gonarthrosis.
- Dystrophic foot diseases.
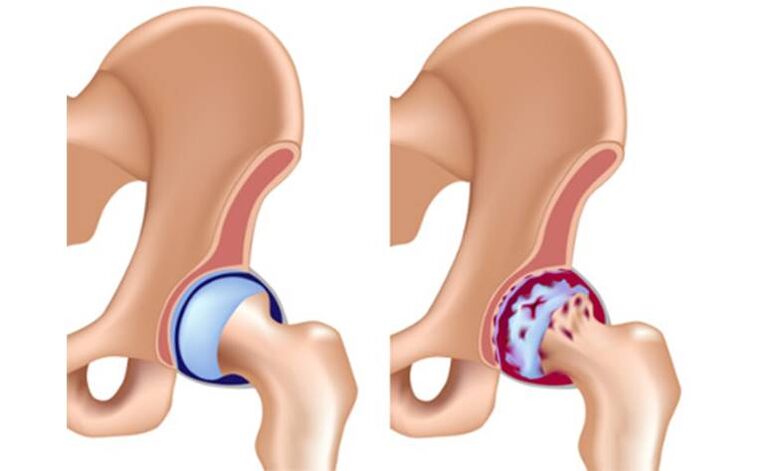
Coxarthrosis
Coxarthrosis is a common and dangerous disease. Initially, a person pays attention to such symptoms as pain in the joints, crunching, clicking when walking. This is all temporary and does not affect quality of life much. As the disease progresses, stiffness worsens and difficulty occurs when attempting to abduct or adduct the leg.
Joint pain can be excruciating, debilitating and bother you at any time of the day. In the morning, my movements are constrained, I have to do exercises for the hip joints in order to spread myself.
Gonarthrosis

Throughout life, the knees experience loads that far exceed a person's weight. This inevitably leads to the development of degenerative processes. If a person suffers from obesity of at least the first or second degree, the deformation of the knees will occur much faster. In the third and fourth years, osteoarthritis deformans is more likely to develop at a young age.
Osteoarthritis of the knee joints has its own characteristics. Why does joint pain occur so often in this area? In addition to the proliferation of bone spurs and degeneration of cartilage, calcium crystals are deposited in the joint cavity. A sort of calcification deposit forms. This condition is called calcium pyrophosphate crystal deposition.
They are first found only in the thickness of the cartilage, then on its surface, in the joint cavity, the tendons and even the muscles.
The deposition of calcium crystals aggravates the progression of deforming osteoarthritis. The disease manifests itself as aching pain, which can turn into sharp pain when the calcification is pinched. Leg mobility is significantly limited. In the knees, deformed joint surfaces, bony growths are visible, and dense nodules can be palpated.
Dystrophic changes in the joints of the feet

The joints of the feet are less susceptible to deforming osteoarthritis. An exception is the metacarpophalangeal joint of the first toe. Its deformities occur in almost all people after 55-60 years. In women, it becomes deformed earlier. The reasons for this are the abuse of narrow and uncomfortable heeled shoes.
In addition to the inconvenience and unsightly appearance of a deformed finger, a person experiences severe pain in the joints. As osteophytes develop, protruding bones form around the toe, making it difficult to wear even wide shoes. Constant injury to osteophytes causes inflammation of the toe joints - polyarthritis develops. The situation can be complicated by the addition of an infection.
Inflammatory diseases of the musculoskeletal system

Inflammation of the joints, affecting several groups of joints at once, is called polyarthritis. If only one joint is inflamed, this form will be called monoarthritis. The symptoms will depend on the type of inflammation or infection that caused it:
- Articular pain.It is often acute – burning or shooting. If the cause of arthritis is an infection, the inflammation becomes purulent. In this case, the pain will be throbbing and very strong. In chronic and subacute forms, joint pain will resemble the variant with osteoarthritis.
- Change shape.In an acute process, an inflammatory tumor forms in the joint area, the skin color changes and the temperature rises. If a bacterial infection occurs, general symptoms of intoxication appear - high fever, chills and health deteriorates sharply. The disease is particularly difficult to tolerate in cases of polyarthritis.
- Impaired function.Movement in an inflamed joint is significantly limited due to pain and fluid buildup in the joint cavity. This swelling, like an inflammatory tumor, mechanically prevents movement.
Causes of arthritis
The causes of arthritis are varied. These diseases are generally divided into main groups:
- Infectious.They develop when the joint is directly affected by an infection, such as Lyme disease. The infection can be viral or bacterial, entering from the outside or from a neighboring affected organ, the bone. Arthritis caused by a bacterial infection is particularly serious.
- Reagent.In this case, the inflammatory process develops in reaction to a past or present infection. These include damage to the musculoskeletal system after flu, colds and urogenital infections. An important sign is the connection with infection.
- Autoimmune.Sometimes a person's immune system begins to destroy its own cells. The manifestations of these diseases are varied, but the joint syndrome is usually the most clearly expressed. The most common autoimmune pathology is rheumatoid arthritis. It is characterized by severe deformation of the joints accompanied by persistent pain.
Autoimmune polyarthritis cannot be cured, but it must be stopped in order to keep the disease at an early stage.
Treatment of joint diseases

What to do if you are diagnosed with a joint disease? Should I take medications, antibiotics or can I limit myself to folk remedies? Only a doctor can answer all questions correctly and he will prescribe the appropriate treatment.
ethnoscience
Folk remedies have been prescribed for a long time, both by modern healers and doctors. They are quite capable of relieving inflammation and eliminating pain, thereby reducing swelling in the affected area.
Among folk remedies, cabbage leaf is considered the undisputed leader. Applying it cold or in a compress with honey to a painful joint can relieve inflammatory manifestations and alleviate the disease. Plantain leaves, chopped mushrooms and vodka liqueurs are also used.
The arsenal of folk remedies is varied, but you need to remember that they can only treat mild forms of diseases and always under the supervision of a doctor.
Drugs

Drugs used in the treatment of joint diseases are aimed at all stages of the pathological process. Main groups of drugs:
- Analgesics and anti-inflammatories.These are usually drugs from the same group. Since the main symptom of joint diseases is pain, relieving it is the doctor's first priority. A good effect is achieved by using local remedies.
- Steroid and cytostatic hormones.It is strictly forbidden to take these medications without a medical prescription. They are used for all serious autoimmune processes and are designed to relieve specific inflammation in the body. Without hormonal drugs, it is impossible to get rid of pain and inflammatory tumor associated with rheumatoid arthritis. They also inhibit joint deformities.
- Antibiotics.They are prescribed if the cause of arthritis is a bacterial infection. Broad-spectrum antibiotics are used and penetrate well into bone tissue. Sometimes, if the pathogen persists, the doctor may treat the infection using several groups of antibiotics. This is also justified if the disease is caused by a mixed infection. It should be remembered that antibiotics are powerful drugs with individual side effects and one should strictly follow the doctor's instructions during the treatment process.
- Preparations that protect and restore cartilage.It is impossible to treat chronic polyarthritis and deforming osteoarthritis without chondroprotectors. For this purpose, single drugs - chondroitin or glucosamine - and combined drugs are used. There is ample evidence on the use of chondroprotectants, based on numerous clinical trials.
- Intra-articular injections.This is the best way to deliver the medication directly to the site of disease. Typically, hormonal anti-inflammatory drugs are injected into the joint cavity. In recent years, hyaluronic acid has also been used as an intra-articular injection.
Physiotherapy

It is not worth treating joint diseases only with medications. The integrated use of physiotherapeutic techniques (magnetotherapy, electrophoresis) and physiotherapy significantly increases the chances of recovery.
Orthopedic devices are also used to limit movement of affected joints. These include orthotics and splints. The purpose of these devices is to reduce the load on the diseased joint.
Surgical treatment
Endoprostheses constitute a radical cure for advanced osteoarthritis. Only this method is capable of replacing a destroyed joint with a synthetic joint, thus restoring its full range of movement.
Stent replacement is a therapeutic option in situations where conservative treatment is powerless.































